Telehealth Visits: Keeping Up with the Latest Changes
July 31, 2023
Now that the public health emergency is officially over, some of the coding requirements regarding telehealth visits that were put in place during the COVID-19 pandemic have been revised. To receive reimbursement for these visits, your billing will need to reflect the changes that went into effect on June 1, 2023. Let’s take a closer look at what has changed this week.
Permanent Medicare Changes:
- Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) can now serve as distant site providers for behavioral/mental telehealth services.
- Medicare patients are now eligible to receive telehealth services for behavioral/mental health care in the comfort of their homes.
- There are no geographic restrictions for the originating site for behavioral/mental telehealth services.
- Behavioral/mental telehealth services can now be delivered using audio-only communication platforms.
- Rural Emergency Hospitals (REHs) are now eligible originating sites for telehealth services.
Temporary Medicare Changes through December 31, 2024:
- FQHCs and RHCs are now allowed to serve as distant site providers for non-behavioral/mental telehealth services.
- Medicare patients are eligible to receive telehealth services in the comfort of their own homes.
- There are no longer any geographic restrictions on the originating site for non-behavioral/mental telehealth services.
- Some non-behavioral/mental telehealth services can now be delivered using audio-only communication platforms.
- An in-person visit within six months of an initial behavioral/mental telehealth service, and annually thereafter, is no longer required.
- Telehealth services can now be provided by all eligible Medicare providers.
You can find the detailed changes outlined by the U.S. Department of Health and Human Services at this link: https://telehealth.hhs.gov/providers/telehealth-policy/policy-changes-after-the-covid-19-public-health-emergency
Source: Consolidated Appropriations Act, 2023
So, what do these changes mean for charge submittals?
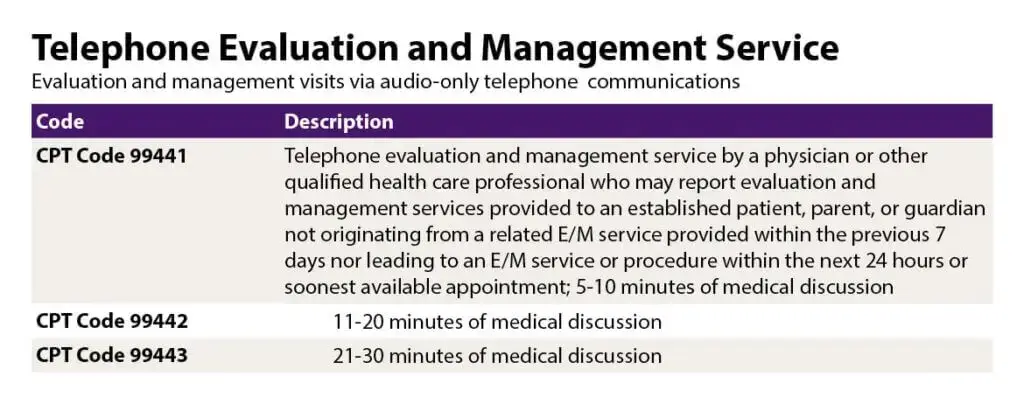
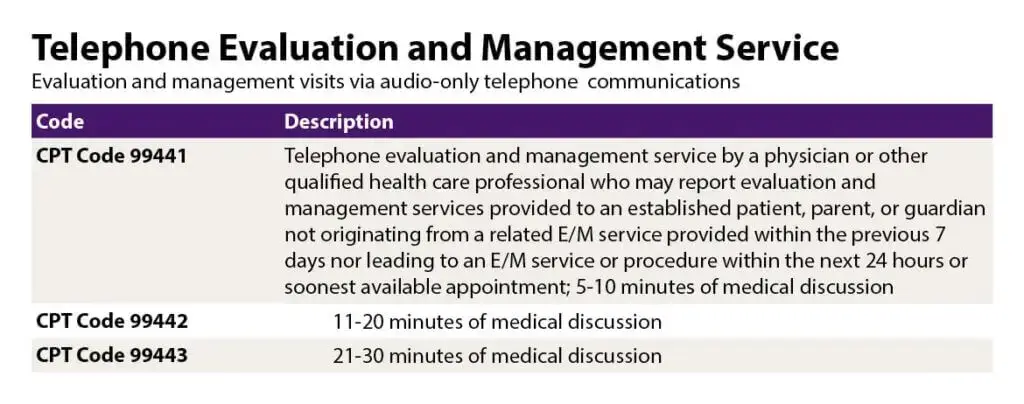
For family/pediatric/Internal medicine offices, the CPT codes remain the same. The CS modifier is no longer used; the 93 and 95 modifiers still depend on the individual Insurance companies’ guidelines and policies. Medicare-allowable, audio-only telehealth services still require FQ.
As of 6/6/2023:
https://www.ama-assn.org/practice-management/digital/ama-telehealth-policy-coding-payment
Documentation requirements for telehealth visits remain the same. They must include:
-
- Date of service
- Patient ID number
- Patient-informed consent
- Location of the physician
- Location of the patient
- Method of communication (audio only / video and audio)
- Exact time spent on the call
- Reason for call / chief complaint
- Diagnosis and impression
- Evaluation results and recommendations
Confused about the 2023 medical coding changes?
Register for our Mid-year E/M Coding Check-up Webinar!
Reserve your spot now: https://bit.ly/43lsWWZ
Boost your revenue cycles with the knowledge and insights
shared by Nancy Entwistle, one of our medical coding experts.
|
|
Michelle Sergei-Casiano CPC, CFPC, CEMC Senior Manager, Regulatory and Coding Compliance coders@calmwatersai.com |