by Kevin Lewis, Former CFO, Physician Housecalls
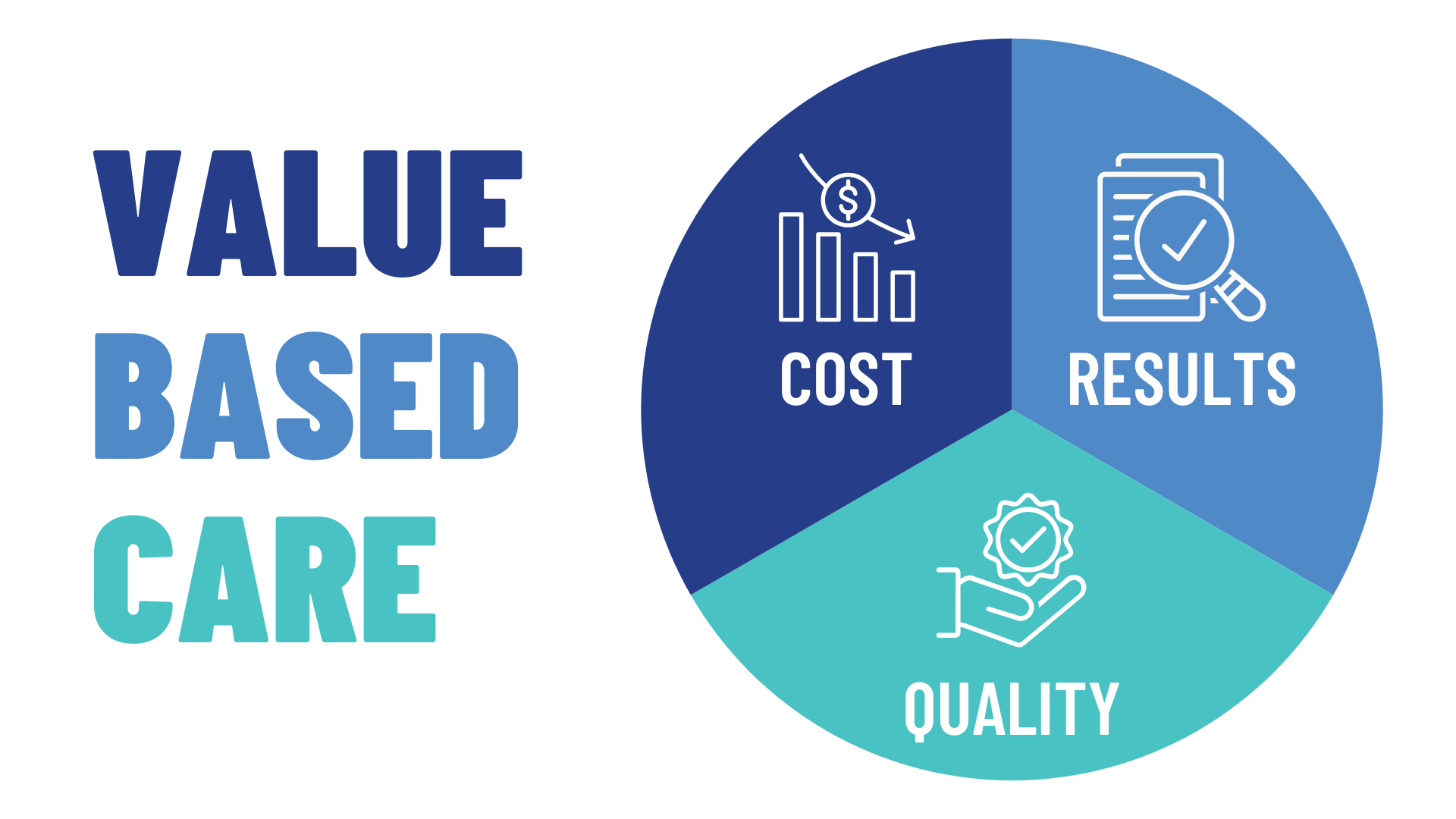
You may be hearing the terms ( or their acronyms) “value-based care” (VBC), “accountable care organizations” (ACOs), “benchmarks,” “shared savings,” and other new phrases that leave you scratching your head about what they mean and how they impact healthcare.
I hope to provide some clarity here. But, first, a little background for context.
Historically, healthcare providers have been reimbursed by public and private insurance payorsthrough fee-for-service arrangements based, as the name suggests, on the services they deliver to patients. The more services they provide, the more fees they receive. The volume of patient visits and type of services provided drive overall practice revenue.
You may have noticed what is missing in this reimbursement model: the “value” generated by the care, driven by the overall quality of the services provided. Let’s walk through a hypothetical example to illustrate the point.
Ms. Jones sees Provider A for an issue. Provider A doesn’t use the most up-to-date treatment guidelines, so Ms. Jones has to return three times for additional treatment (a total of four visits).
Mr. Smith sees Provider B for the same issue as Mrs. Jones. Because Provider B uses the most up-to-date treatment guidelines and follows up with calls, Mr. Smith only needs one visit for effective treatment.
Under fee-for-service reimbursement, Provider A’s out-of-date treatment approach results in payments for four visits, while Provider B, who delivered effective care more efficiently, gets paid for only one visit. Doesn’t that seem backwards?
Most of us, I think, would agree that Provider B delivered better quality of care since the treatment was effective and the patient did not have to return for additional visits. And since Provider B’s care achieved the same outcome as Provider A’s care but required only one visit rather than four, the “value” of Provider B’s care is higher than that of Provider A. Put another way, the ‘value’ of Provider A’s care is four times lower than Provider B’s services.
Value-based care attempts to address this disparity incentivized by fee-for-service models by rewarding practitioners like Provider B, who deliver high-quality care at a low cost, and by punishing practitioners like Provider A, who cost the health system more money due to low-quality care requiring numerous visits or other expensive interventions.
You’re probably wondering how this works in the real world, since it’s tough to know ahead of time who falls into the ‘Provider A’ group and who is in the ‘Provider B’ group. This is where Accountable Care Organizations and benchmarks enter the conversation.
An accountable care organization (ACO) works with groups of providers to hold them ‘accountable’ for the overall cost of caring for their patients. How does it work? First, the providers measure the cost they incur to care for patients today (i.e., the cost of all the visits, tests, x-rays, medications, etc.). Then they compare this amount with their ‘benchmark’ cost of care—the actual costs incurred in caring for their patients in the past.
To promote lowering costs from year to year, the ACO shares some of the savings the providers generate from one year to the next by improving care quality. These “shared savings” incentivize providers to deliver more effective care rather than more care. Here’s an example:
Let’s say Accountable Care Organization X has ten practices in its group. Last year, the average cost of care (the benchmark) was $1,000 per patient per year. To encourage higher quality of care this year, ACO X tells the ten practices that they will earn 50% of any savings from last year’s $1,000 benchmark. At the end of the year, the practices reduced their total cost of care to $800 per patient—a savings of $200 from the benchmark—so they receive $100 per patient as their share of that savings. The practices are incentivized because they can receive $100 more per patient than it costs them to deliver care.
While it takes some time to digest these terms and these models work, the shift toward value-based care reimbursement continues to accelerate. According to a 2023 survey from The Commonwealth Fund, 30% of primary care physicians said their practices receive at least some of their revenue from a shared savings model. That amount will only grow—and quickly. CMS has announced its intent to shift all Medicare, Medicare Advantage, and Medicaid payments to value-based models by 2030. So the sooner you prepare, the better positioned you’ll be to take advantage of the shift.
Kevin Lewis is Senior Vice President, Finance and Value-Based Care for Calm Waters AI and formerly served as Chief Financial Officer for Physician House Calls, a large specialty provider group headquartered in Oklahoma.
Ready to enhance revenue cycle performance and help ensure that providers’ medical documentation is complete and “bulletproof” before it leaves their desktops? View a demo of Calm Waters AI and learn more about our documentation improvement services with ChartPal.